Τα τελευταία χρόνια το ενδιαφέρον της επιστημονικής κοινότητας έχει στραφεί προς μια επιπλοκή του διαβήτη, την υπογλυκαιμία.
Αν ο διαβήτης αποτελεί την μεταβολική μάστιγα του καιρού μας, η υπογλυκαιμία αποτελεί την πιο άμεσα απειλητική για τη ζωή επιπλοκή του. Είναι μια οξεία κατάσταση που πρέπει να αντιμετωπίζεται από τον ίδιο τον ασθενή και τους ανθρώπους που βρίσκονται κοντά του κατά την εκδήλωσή της. Επομένως, η καλή ενημέρωση, το σωτήριο αυτό «φάρμακο» σε όλες τις επείγουσες περιπτώσεις δεν αφορά μόνο τους πάσχοντες αλλά κυριολεκτικά τον καθένα μας, αφού μπορεί να μας βοηθήσει να βοηθήσουμε τη ζωή να συνεχίσει, αναφέρει η Αικατερίνη Ν. Τρικκαλινού, MD, PHD C,Παθολόγος – Διαβητολόγος, Επιμελήτρια Διαβητολογικού – Καρδιομεταβολικού Κέντρου Metropolitan Hospital.
Η υπογλυκαιμία αποτελεί μια οξεία επιπλοκή του διαβήτη. Τα τελευταία χρόνια εστιάζεται πάνω της ολοένα και περισσότερο το επιστημονικό ενδιαφέρον, καθώς οι γνώσεις μας στο εν λόγω θέμα αυξάνονται και αναγνωρίζονται οι βραχυπρόθεσμες όσο και οι μακροπρόθεσμες συνέπειές της. Σήμερα είναι σαφές το γεγονός πως οι ασθενείς που υφίστανται υπογλυκαιμικά επεισόδια κινδυνεύουν περισσότερο από εκείνους που δεν κάνουν τέτοια επεισόδια. Στη συγκεκριμένη ομάδα και συγκριτικά με τον υπόλοιπο πάσχοντα πληθυσμό, ο κίνδυνος για εμφάνιση καρδιαγγειακού επεισοδίου, εμφράγματος ή αγγειακού εγκεφαλικού επεισοδίου, ή θανάτου (MACE) οκταπλασιάζεται μία εβδομάδα μετά από επεισόδιο σοβαρής υπογλυκαιμίας και παραμένει διπλάσιος για χρονικό διάστημα μεγαλύτερο του έτους μετά το συμβάν, όπως φάνηκε από την ανάλυση της μελέτης LEADER. Επίσης, από την ίδια μελέτη, γνωρίζουμε πως ο κίνδυνος για θνητότητα από όλες τις αιτίες δεκαπλασιάζεται μετά από ένα σοβαρό υπογλυκαιμικό επεισόδιο και παραμένει διπλάσιος για χρονικό διάστημα μεγαλύτερο του ενός έτους μετά το συμβάν. Δυστυχώς δεν είναι λίγα τα περιστατικά θανάτων ηλικιωμένων όσο και νεαρών ατόμων από υπογλυκαιμία ακόμα και σήμερα παρόλο που η νέα βιοτεχνολογία των ινσουλινών και τα νέα αντιδιαβητικά δισκία έχουν μειώσει σημαντικά τα επεισόδια υπογλυκαιμίας.
Τι είναι υπογλυκαιμία
Σύμφωνα με τις κατευθυντήριες οδηγίες της Ελληνικής Διαβητολογικής Εταιρείας (2018) ως υπογλυκαιμία ορίζεται η κατάσταση κατά την οποία η γλυκόζη πλάσματος είναι χαμηλότερη των 70mg/dl με ή χωρίς συμπτώματα.
Αιτίες της υπογλυκαιμίας
• Καθυστέρηση λήψης γεύματος
• Παράλειψη γεύματος
• Μειωμένη ποσότητα γεύματος
• Δίαιτα αδυνατίσματος
• Νευρογενής ανορεξία
• Ασυνήθιστη σωματική κόπωση
• Λήψη οινοπνεύματος
• Ακατάλληλες δόσεις και τύπος ινσουλίνης
• Πολύ αυστηρή ρύθμιση διαβήτη
• Ενδοκρινικές ανεπάρκειες
• Μειωμένη αντιρρόπηση γλυκόζης
• Μειωμένη αντίληψη υπογλυκαιμίας
• Διακοπή κορτικοστεροειδών
• Νεφρική ανεπάρκεια
• Θηλασμός
• Γαστροπάρεση, έμετοι
• Σύνδρομο δυσαπορρόφησης
• Μειωμένη αντίληψη οδηγιών ιατρού.
Συμπτώματα της υπογλυκαιμίας
Α) Αδρενεργικά (εξαιτίας διέγερσης του αυτόνομου νευρικού συστήματος): εφίδρωση, άγχος, περιχείλιες αιμωδίες, ναυτία αίσθημα θερμότητας, ταχυκαρδία, αίσθημα παλμών και τρομώδεις κινήσεις.
Β) Νευρογλυκοπενικά (εξαιτίας μειωμένης τροφοδοσίας του εγκεφάλου σε γλυκόζη): κεφαλαλγία, ελάττωση συγκέντρωσης, δυσαρθρία, διαταραχή της συμπεριφοράς, σύγχυση, υπνηλία, λήθαργος, ρίγος, παροδική ημιπληγία, αφασία, σπασμοί, κώμα.
Συμπτώματα της υπογλυκαιμίας
Συμπτώματα της υπογλυκαιμίας
Γ) Μη ειδικά ̶ αταξινόμητα: πείνα, αδυναμία, διπλωπία, θάμβος οράσεως.
Είναι εξαιρετικά σημαντικό να τονιστεί ότι τα συμπτώματα της υπογλυκαιμίας διαφοροποιούνται με την ηλικία. Στην παιδική ηλικία προεξάρχει η αλλαγή συμπεριφοράς, στη μέση ηλικία εμφανίζονται τα συμπτώματα που περιγράφτηκαν παραπάνω, ενώ στην τρίτη ηλικία προεξάρχουν τα νευρολογικά συμπτώματα που συχνά δυσκολεύουν τη διάγνωση (διαταραχές όρασης, διαταραχές ισορροπίας, έλλειψη συντονισμού κινήσεων). Επίσης, η αντίληψη των συμπτωμάτων της υπογλυκαιμίας μπορεί να επηρεάζεται, να εμποδίζεται ή να τροποποιείται από μια πλειάδα παραγόντων όπως: ο ύπνος, η απόσπαση της προσοχής (για παράδειγμα κατά την εργασία του ασθενούς), η στάση του σώματος, φάρμακα, αλκοόλ, ψυχολογικοί παράγοντες, ή άγνοια των συμπτωμάτων της υπογλυκαιμίας. Τέλος, πολύ σημαντικό είναι να αναφερθεί ότι τα συμπτώματα της υπογλυκαιμίας διαφοροποιούνται όχι μόνον από άνθρωπο σε άνθρωπο αλλά και από υπογλυκαιμικό επεισόδιο σε υπογλυκαιμικό επεισόδιο και, φυσικά, αλλάζουν με την πάροδο του χρόνου και τη διάρκεια του διαβήτη και τα επανειλημμένα επεισόδια υπογλυκαιμίας.
Κατηγορίες υπογλυκαιμίας
Ελαφρά-ήπια υπογλυκαιμία: δίνει ήπια συμπτώματα υπογλυκαιμίας τα οποία μπορεί να είναι εφίδρωση ταχυκαρδία και αίσθημα κόπωσης και μπορεί να διαλάθουν της προσοχής του ασθενούς.
Κλινικά σημαντική υπογλυκαιμία: ως τέτοια ορίζεται η κατάσταση κατά την οποία η γλυκόζη πλάσματος είναι χαμηλότερη από 54mg/dl.
Σοβαρή υπογλυκαιμία: αυτή είναι η υπογλυκαιμία (ανεξαρτήτως επιπέδου γλυκόζης) κατά την οποία ο ασθενής χρειάζεται βοήθεια από άλλους για να τη διορθώσει και να αποκτήσει πλήρως την επαφή του με το περιβάλλον. Επίσης, κατ` άλλους συγγραφείς, σημαντική είναι η χρήση των όρων κλινική υπογλυκαιμία, όταν υπάρχουν συμπτώματα και σημεία υπογλυκαιμίας που ανατάσσονται με τη χορήγηση γλυκόζης, βιοχημική υπογλυκαιμία όταν τα επίπεδα της γλυκόζης πλάσματος είναι κάτω των 70mg/dl (ή κατ` άλλους συγγραφείς κάτω των 58mg/dl ή κάτω των 50mg/dl εάν πρόκειται για φλεβικό αίμα). Στην τελευταία αυτή κατηγορία υπογλυκαιμίας, στο 40%των ασθενών δεν υπάρχουν τα υποκειμενικά συμπτώματα υπογλυκαιμίας, δηλαδή, οι εν λόγω ασθενείς έχουν παθολογικά μειωμένη αντίληψη της υπογλυκαιμίας. Μιλάμε για ανεπίγνωστη υπογλυκαιμία ή έλλειψη επίγνωσης της υπογλυκαιμίας, όταν οι ασθενείς είτε δεν αντιλαμβάνονται την υπογλυκαιμία είτε, όταν εμφανίζουν τα συμπτώματα, έχουν ήδη νευρογλυκοπενία και γι` αυτό δεν τα αντιλαμβάνονται. Αυτή αφορά το 20%-25% των ασθενών με ινσουλινοεξαρτώμενο διαβήτη τύπου 1 και το 10% των ασθενών με μη ινσουλινοεξαρτώμενο διαβήτη τύπου 2 στους οποίους ο κίνδυνος εμφάνισης σοβαρής υπογλυκαιμίας εξαπλασιάζεται. Είναι, επίσης, πολύ σημαντικό να σημειωθεί πως η ανεπίγνωστη υπογλυκαιμία αντιμετωπίζεται και αναστρέφεται με κατάλληλη εκπαίδευση του ασθενούς ούτως ώστε να περιοριστούν τα υπογλυκαιμικά επεισόδια και να βελτιωθεί η αντίληψη των συμπτωμάτων της υπογλυκαιμίας. Τέλος, ιδιαίτερη μνεία πρέπει να γίνει στη νυκτερινή υπογλυκαιμία, καθώς οι ασθενείς κατά τη διάρκεια της νύχτας δεν κάνουν τον συνήθη αυτοέλεγχο και δεν είναι σε εγρήγορση, τα δε συμπτώματα μπορεί να μην είναι κατανοητά. Αυτά μπορεί να είναι ανήσυχος ύπνος, εφιάλτες, πρωινή κεφαλαλγία, αίσθημα κόπωσης κατά την αφύπνιση, ανεξήγητη υπνηλία, εσώρουχα υγρά από ιδρώτα.
Αντιρρόπηση υπογλυκαιμίας:
Σε μη διαβητικά άτομα
Η ελάττωση των επιπέδων της γλυκόζης σε φυσιολογικά άτομα έχει τις ακόλουθες συνέπειες (αντιστοιχισμένες απόλυτα με τα συγκεκριμένα επίπεδα γλυκόζης πλάσματος).
1. Μείωση της έκκρισης ινσουλίνης από τα β κύτταρα (γλυκόζη 80mg/dl).
2. Αύξηση της γλυκαγόνης και της αδρεναλίνης (γλυκόζη 69mg/dl).
3. Αύξηση της κορτιζόλης και της αυξητικής ορμόνης καθώς και άλλων νευρομεταφορέων (γλυκόζη 67mg/dl).
4. Εμφάνιση νευρογενών-αδρενεργικών συμπτωμάτων (γλυκόζη55mg/dl).
5. Εμφάνιση νευρογλυκοπενικών συμπτωμάτων (γλυκόζη 50mg/dl).
6. Διαταραχές νοητικών λειτουργιών (γλυκόζη 46 mg/dl).
Σε διαβητικά άτομα
Οι προαναφερθέντες μηχανισμοί αντιρρόπησης διαταράσσονται στα άτομα με διαβήτη. Έτσι σε «αρρύθμιστους» ασθενείς (με αρρύθμιστο διαβήτη) τα επίπεδα γλυκόζης μετακινούνται σε υψηλότερες τιμές, ενώ σε «ρυθμισμένους» σε αυστηρά επίπεδα ασθενείς είναι δυνατό να μετακινηθούν σε χαμηλότερες τιμές.
Οι άμεσοι κίνδυνοι της υπογλυκαιμίας
Η υπογλυκαιμία έχει πολλές άμεσες συνέπειες. Διαταραχές του θυμικού, κατάθλιψη, σπασμούς, κώμα, ελαττωμένες εργασιακές επιδόσεις, επικίνδυνη οδηγική συμπεριφορά, τροχαία ατυχήματα, πτώσεις στο έδαφος, κατάγματα, τραυματισμούς, οξέα συμβάματα (καρδιακή ισχαιμία, αγγειακό εγκεφαλικό επεισόδιο, έμφραγμα, αρρυθμίες, ανακοπή θάνατο).
Οι μακροπρόθεσμοι κίνδυνοι της υπογλυκαιμίας
Μακροπρόθεσμα, οι συχνές υπογλυκαιμίες μπορεί να προκαλέσουν προβλήματα στην εργασιακή ζωή των ασθενών (απόλυση, ανεργία), δυσκολία στην απόκτηση άδειας οδήγησης ή απώλεια αυτής, μειωμένη ποιότητα ζωής, διαταραχές στις διαπροσωπικές σχέσεις, φόβος, ελλειμματική συμμόρφωση στη θεραπεία του διαβήτη, γνωσιακή έκπτωση, άνοια, μειονεκτική αντιρρόπηση της υπογλυκαιμίας, ανεπίγνωστη υπογλυκαιμία.
Αντιμετώπιση υπογλυκαιμίας
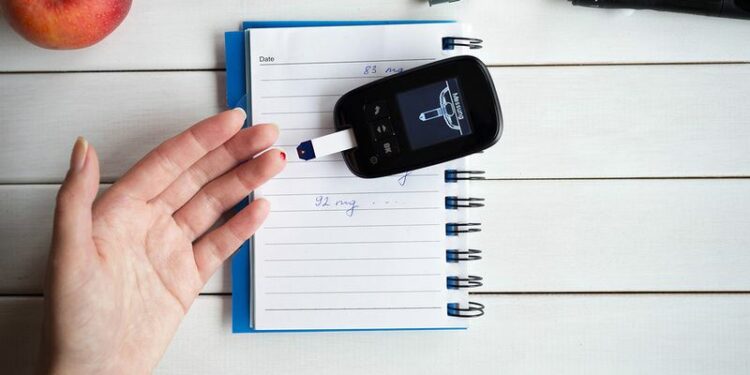
Η Αντιμετώπιση της υπογλυκαιμίας θα πρέπει να γίνεται αμέσως, γιατί κινδυνεύει η ζωή του ασθενούς. Εάν είναι δυνατόν πρέπει να γίνεται μέτρηση σακχάρου αίματος για να πιστοποιηθεί η υπογλυκαιμία. Αν δεν είναι δυνατόν ή δεν υπάρχει άλλο πρόσωπο να βοηθήσει πρέπει ο ασθενής να προχωρήσει σε άμεση λήψη γλυκόζης, π.χ., μισό ποτήρι χυμού φρούτων, ή τρία χάπια γλυκόζης ή μια συσκευασία ζελέ γλυκόζης ή 5-6 σκληρές καραμέλες. Μετά από 15 λεπτά πρέπει να γίνεται επανέλεγχος της γλυκόζης. Εάν τα επίπεδα σακχάρου εξακολουθούν να είναι χαμηλά επαναλαμβάνουμε τη λήψη σακχαρούχου υγρού και ακολουθεί λήψη κανονικού γεύματος ή σνακ (προσοχή: τα σκευάσματα που λαμβάνονται για τη διόρθωση της υπογλυκαιμίας να μην είναι υγρά, ζελέ ή καραμέλες χωρίς ζάχαρη). Τα λοιπά γλυκά, για παράδειγμα η σοκολάτα, τα κρουασάν, τα μπισκότα λόγω μεγάλης περιεκτικότητας σε λίπος (το λίπος επιβραδύνει την απελευθέρωση της γλυκόζης από το έντερο στο αίμα) είναι ακατάλληλα για την άμεση αντιμετώπιση της υπογλυκαιμίας.
Μέτρα πρόληψης της υπογλυκαιμίας
1. Συχνά γεύματα: έξι γεύματα την ημέρα προσαρμοσμένα στις ανάγκες των ασθενών. Πρωινό, δεκατιανό, μεσημεριανό απογευματινό, βραδινό και γευματίδιο προ του ύπνου (εξαιρετική η σημασία του στην πρόληψη των νυκτερινών υπογλυκαιμιών).
2. Αποφυγή καθυστέρησης λήψης γεύματος (ιδίως όταν χρησιμοποιούνται μίγματα ινσουλινών).
3. Ορθολογικός αυτοέλεγχος, με μετρήσεις σακχάρου αίματος. Ιδιαίτερα εάν, προ ύπνου, η γλυκόζη αίματος είναι χαμηλότερη από110 mg/dl τότε επιβάλλεται λήψη υδατανθρακούχου γευματιδίου.
4. Αποφυγή σωματικής εξάντλησης ή μεγάλης κόπωσης.
5. Τακτικός έλεγχος συννοσηροτήτων.
Τι από τα παραπάνω επιβάλλεται να ξέρει ο ασθενής φεύγοντας από το διαβητολογικό ιατρείο;
Ο ασθενής στον οποίο έγινε διάγνωση διαβήτη, ιδιαιτέρως διαβήτη τύπου 1, πρέπει, οπωσδήποτε, μαζί με τη διάγνωση, να ενημερωθεί και, ει δυνατόν, να εξοικειωθεί (να γνωρίσει τόσο ώστε να μπορεί να αντιμετωπίσει) τα παρακάτω:
• Τι είναι υπογλυκαιμία
• Ποια είναι τα όρια της υπογλυκαιμίας
• Ποια είναι τα συμπτώματα της υπογλυκαιμίας
• Τι πρέπει να κάνει εάν έχει υπογλυκαιμία
• Πώς θα αποτρέψει μια μελλοντική υπογλυκαιμία.
Πηγή: iefimerida.gr